Contents Plus [hide]
Innovations on my watch
All governors are different with varying backgrounds and experiences. Many have a strong urge to improve their Trust’s delivery of services, but this is the role of the Board and Management and not for the Governors. They are there to scrutinize! When I joined the Council I recognised that there was a role for me in innovating; not in delivery of Trust services, but in execution of governors’ processes. To make the Governors’ work more effective.

It is hard, almost impossible, to work alone as a governor. On the one hand governors are a potential thorn in the side of senior management – cooperation from the Trust is desirable for most things, but cannot be taken for granted. On the other hand much governor activity by its very nature is collegiate. Some of the matters discussed here relied much on support from my fellow-governors for which I am grateful.
The Governor’s Voice
There is not enough time in Governors’ Council meeting. Governors ‘hold Trust Management to account’ by asking questions, and there is never enough time! The more management talk – the less time for questions; the more items on the agenda – the less time for questions; the more governors talk – the less time for questions.
What do Governors themselves actually talk about in their Council meetings? Some governors love to talk about themselves – about aircraft safety and maintenance, or their personal NHS care, or to catalogue names of Trust managers they have talked to, or about volunteering activity in other organisations. Some governors want to talk about what they read in the newspapers. Some are focused on healthcare in their community whether it involves the Trust or not. Yet others want to announce events from unrelated organisations. A few look at the papers on the agenda and have questions and analysis of the information provided. Then there’s the majority of governors who say very little.
The Governors Council is a meeting of un-equals. On the one hand is The Management – all experts at their subject and very experienced in meeting behaviours. On the other side, the Governors, with varying backgrounds but mostly without extensive NHS knowledge and without experience of the civil-service bureaucracy which the NHS emulates. The meetings are run by the Chairman of the Trust, but in many ways are controlled by the CEO. The availability of him and his management team usually matches (or limits) the possible flow of useful information to governors.
My predecessor as Lead Governor started a process of soliciting questions for the executive in advance from her fellow-governors by email. This allowed those who found it difficult to intervene in the meeting to ‘book a slot’ at the next meeting. It also gave management pre-warning of the subjects and allowed them to do some homework. It did not work very well. The governor was still expected to articulate their question in the meeting – which made anxious governors less likely to volunteer. Often management failed to gather the necessary information to provide an answer.
This was one of the first jobs I tackled as Lead Governor. We focused on the subject of the question, rather than the person who raised it. And, in response to the CEO’s complaint that all the questions were coming from the same 2 or 3 governors, I made them anonymous. This upset the new Chairman at the time. The issue was eventually resolved with management making written answers so the question, the questioner, and the answer were all published in advance with the meeting papers. This was a good outcome – written answers reduced the time needed for discussion which could then focus on supplementary points.
It is inevitable in a group like this that most of the questions will come from a few individuals who are particularly engaged with the business of the Trust. But I felt that some of the governors had views and concerns, but were shy of raising them in the main meeting. As Lead Governor I attempted to address this by arranging a ‘Governors’ Private Pre-meeting’ which convened 30 or 45 minutes before the main meeting started.

We excluded management and Trust staff from the room and moved chairs into a circle. After some introductory remarks, I went round the room asking each person in turn if they had any points to raise about the forthcoming meeting’s agenda. Then I went round each individual again asking if they had any other issues or concerns they wanted to raise about the Trust. Anyone who tried to talk at length or start a discussion was cut short; there was a sort-of time limit – in practice about 2 minutes. (30 governors using 1 minute each would easily take up the 30 minutes available).
If one of the quieter people raised a concern I thought encouragement from other governors might help them to speak out in the main meeting. It helped to a small degree, but I realised that it was not so much formulating the question, but rather the process of intervening in the main meeting which many people find difficult. To help it was necessary to make an intervention on someone else’s behalf, which I did occasionally. Nevertheless these pre-meetings were popular and they continued to be so when gatherings were forced online during and after Covid.
The pre-meetings were not a place for discussion and, as Lead Governor, I undertook to arrange a supplementary meeting to cover any subject a governor wanted to discuss. My only requirement was that more than one person should want the meeting. This never happened.
Governor credibility
Early on I realised that governors could have a credibility problem with members of the public. I was manning a NHS stand at a local shopping centre and several people asked why the staff had ID cards, but I didn’t. (Maybe I was an imposter! For than matter, did the staff know me?) One person wanted to email information to me and I needed to write down my name and provide him with my personal email address. This happened rarely, but networking and public engagement are an important part of the governor’s role and should be easy to manage. A photo-Id similar to those held by staff, and a business card using the NHS style guide would help!
When I was new a plain white enamel name badge was as far as the Trust went for governor ID. As a member of the Governor Quality group making visits to services, it made sense to me to have a photo-ID that staff and patients could recognise and verify easily. The administration were happy to transfer responsibility for this to the HR department. They insisted on a DBS check as well. Once this was done and I had my card and lanyard my credentials could be recognised both inside and outside the Trust.

The Trust Chairman was keen on us engaging with members of the public and he readily agreed that there should be no obstacle to business cards for governors. The lady in charge of administration had other ideas. Not even her boss, the Company Secretary, has a business card! The Communications Department was responsible for ordering. Their regular supplier would likely charge £100 or more.

After many months of no progress I decided to do it myself. I got hold of the NHS Style Guide. A graphics drawing program was enough to create a suitable card. I made a pictorial design with personal details for the other side. An online print company made 250 double-sided cards for less than £20. Something the NHS bureaucracy would not be able to manage!
Employing Technology for Governors
The governors’ gatekeeper to the Trust was the assistant to the Company Secretary. She was responsible for booking meetings, collating papers, and printing and sending them out as well as supporting The Chair and some of the executive team. She could expect many requests each weeks from governors who had problems with their diaries.
My first contribution was a paper presented at the Membership and Engagement group. I wanted to improve governor communication and independence by using basic IT. My proposal for giving governors Trust email addresses was met by almost universal disdain “the last thing I want is people emailing me about the Trust”! I also wanted an ‘Extranet’ to store documents from past meetings as well as other documents of common interest. And finally an electronic calendar so the admin staff who supported governors could at least be free of repeated enquiries about meeting times.
No-one picked-up any of the ideas or offered support at that time. A shared calendar was something I could tackle myself and I created this using Google software. Eventually, with support from some new governors, staff bought into the idea. They entered governor meetings and important dates for the Trust. Governors, using their phone, could instantly see appointments for them and for Trust management and staff – all colour coded according to who the meetings were for. It also enable location based meetings, for example the Local Authority Healthwatch, to be coded in a different colour separately from personal appointments.

Getting an email address associated with the NHS for governors was not so easy. No objections were raised, but it still took several years for a solution to be proposed by the IT department. Governors were to be kept out of the corporate network, so the only option was the globally available NHS.NET email. Several years later, when Trust IT infrastructure had evolved enough, the conventional email@berkshire.nhs.uk was allowed. Unfortunately security restrictions prevented the integration with personal email. Logging in separately for occasional NHS communication was quite inconvenient.
As governors we are driven by information. And there is a lot of it. All the meetings mentioned in the previous post have associated papers, sometimes hundreds of pages. There is a wide range of resources on Trust Governance and on the NHS produced by NHS-England, by NHS Providers, by research bodies like the The Kings Fund, by charities and other service providers. There are Service Information presentations and guides for Carers and Patients. There are service visit reports from governors detailing governor experiences and perceived shortcomings or stated staff concerns. There are research papers and conference proceedings.
Relevant documents on a subject are assembled for a meeting and then discarded. To refer back required more work from the hard-pressed support staff.
Over many years I lobbied to improve this situation. I maintained my own file system at home and documents distributed electronical found their place in there; but this was only accessible to me. Several meetings with the Head of IT about a governors extranet for documents got nowhere. The Trust technology, the IT knowledge and skills, and the Trust infrastructure was not capable of providing even basic support. After 4 or 5 years the company started work with Microsoft Sharepoint and suddenly we had some resource allocated.
I worked with a governor colleague on the specification of a document store – the way it would be used and the type of information that should be stored alongside each document so it could be readily retrieved. We set up a very simple document database, with basic meta-data. Documents were loaded in the systems and governors could review them by any one of a number of criteria – filtering by meeting type, by service location, or subject matter for example. The success of such a facility depends on keeping the information up-to-date; new meeting papers have to be uploaded all the time. And governors need to be actively engaged with the Trust and interested enough to make use of the facility.
I created the short video above for governors and staff who had “forgotten” how to use the system. The screen image is much clearer in operation and the documents which are displayed here are readily downloaded or enlarge in the App for reading. It is best viewed in full-screen mode – select the outward facing 4 arrows at the bottom of the film. When it ends you may be on a Vimeo screen – use the ‘escape’ key to return to this blog.
What was missing for me was an audit trail of who was using the store. Without feedback it was difficult to feel if this enterprise was successful or not. The truth, I suspect, is that most governors rarely consider the Trust except when they attend a meeting and so the usage of the document store was not high.
Communicating Trust Information
Part of a governor’s job is to evaluate the Trust they are serving. Mostly this depends on information – information that is produced by the Trust and fed to NHS-England, to Management, to Governors, to Staff, and to the Public.
When I became a governor much was difficult to understand. Meeting after meeting I found I needed to ask the same clarification questions. I thought this was a neophyte’s problem, but when I asked other governors they did not understand the figures I was questioning either. Headings which did not describe the item they were related to, obscure NHS 3-letter acronyms, graphs with the axes the wrong way around, colour coding without a key – these were all features of the CEO’s regular performance report to the Governors Council.
It was hard to understand how this could be. The board with its Non-executive Directors would also be scrutinising these figures, so how could they be so difficult and wrong? Eventually the job was passed down the management chain to the department producing the report. I had a series of meetings and email exchanges which fixed most of the problems in the snapshot the governors saw each quarter. When a few figures produced infrequently like this are poor, it leads to concerns about the quality of information organisation wide.
The press and public are very interested in patient wait times. How long after a referral to be seen? How long to receive treatment? From the outset I found it extraordinary that management could not provide wait time figures for services in the Trust. In one or two areas there were targets mandated by government, and these were tracked in some way, but other figures were not. How could members of the board ignore this gaping hole in their management information?
This was a regular information request when I became Chair of the Governors QA group. A bottom-up approach was possible and the manager who supported us could contact different services and try to consolidate the information for our quarterly meetings. For a top-down approach this was raised in discussions with the NEDs and senior management team, and also at Council meetings.
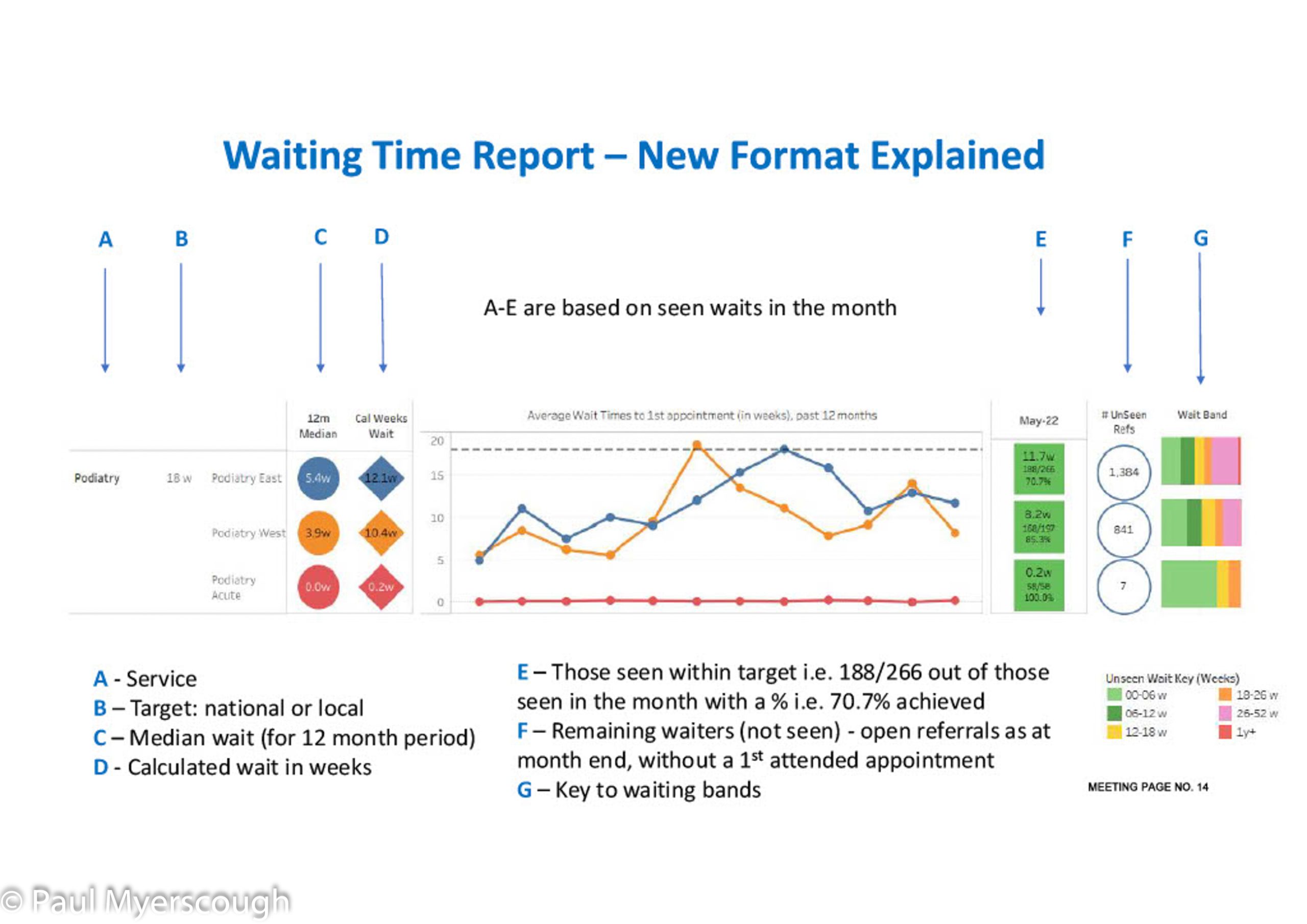
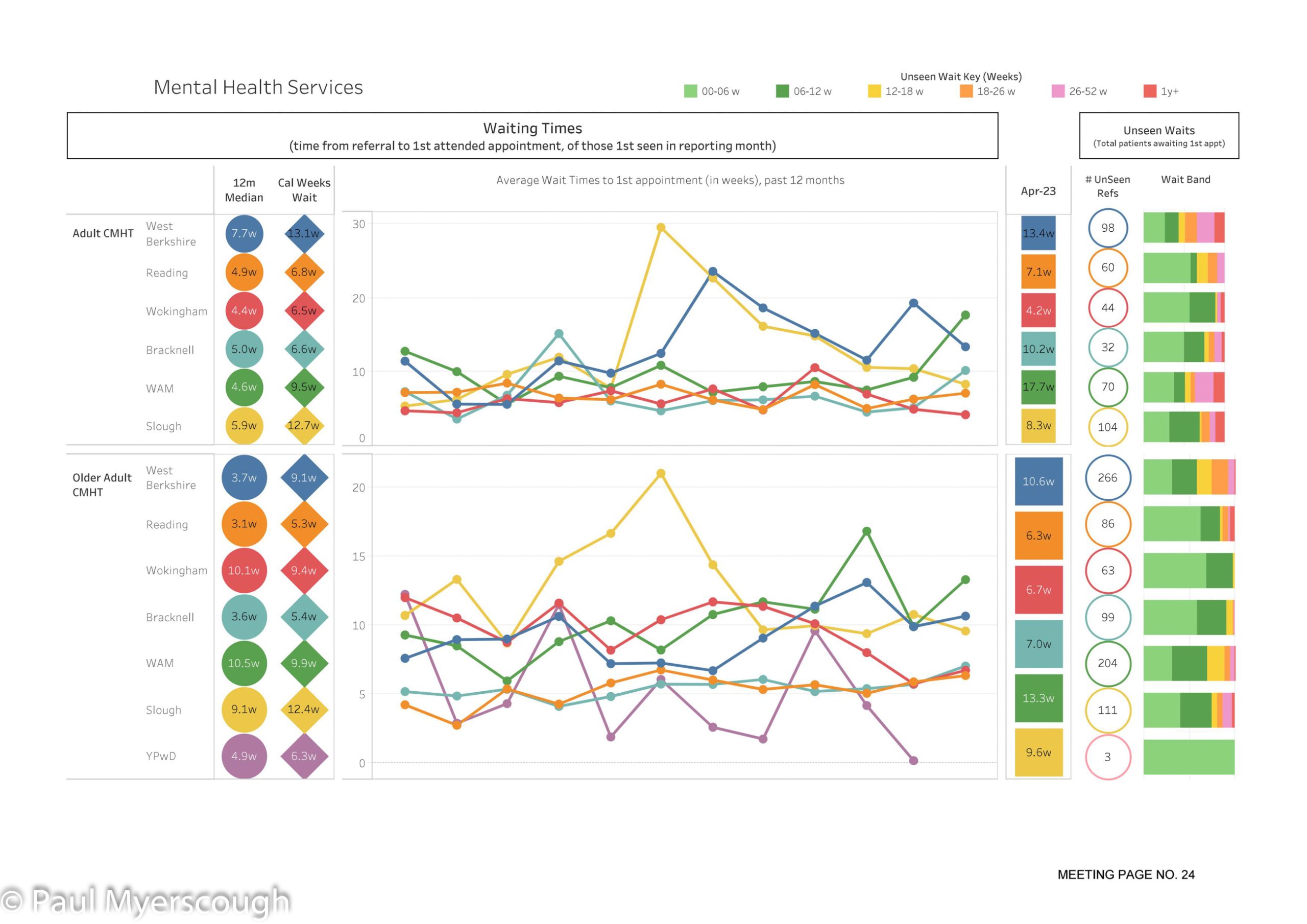
Before long there were one or two other governors that took up the baton too. After 5 or 6 years, and without any warning, my QA meeting was presented with a draft report – full of graphs and colour – which showed some of the statistics we had been waiting for.
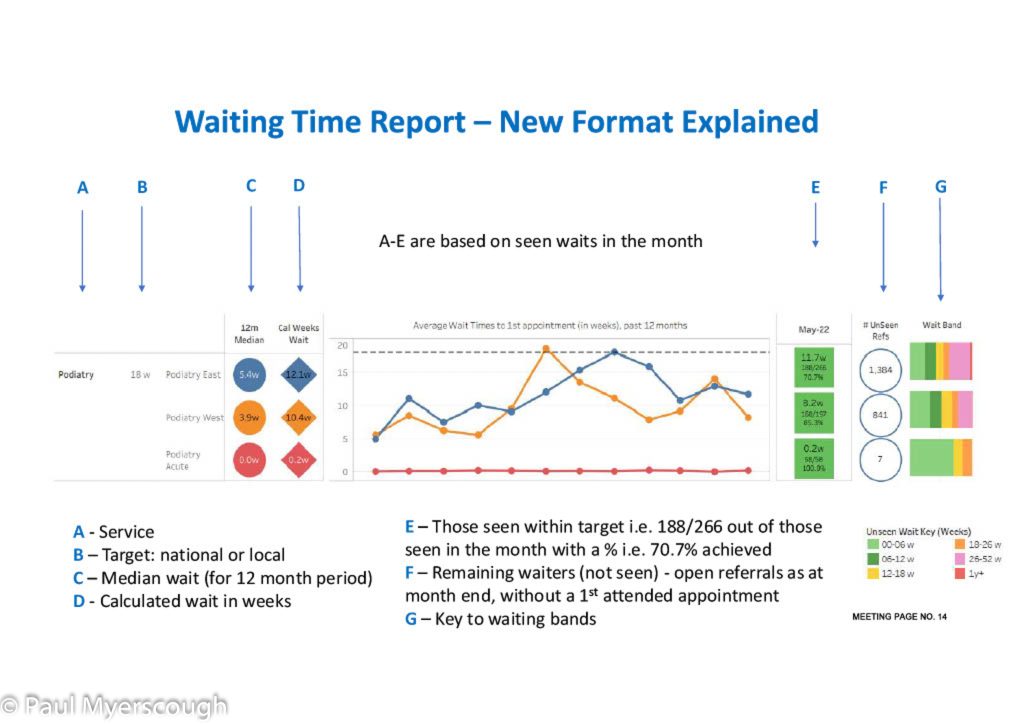
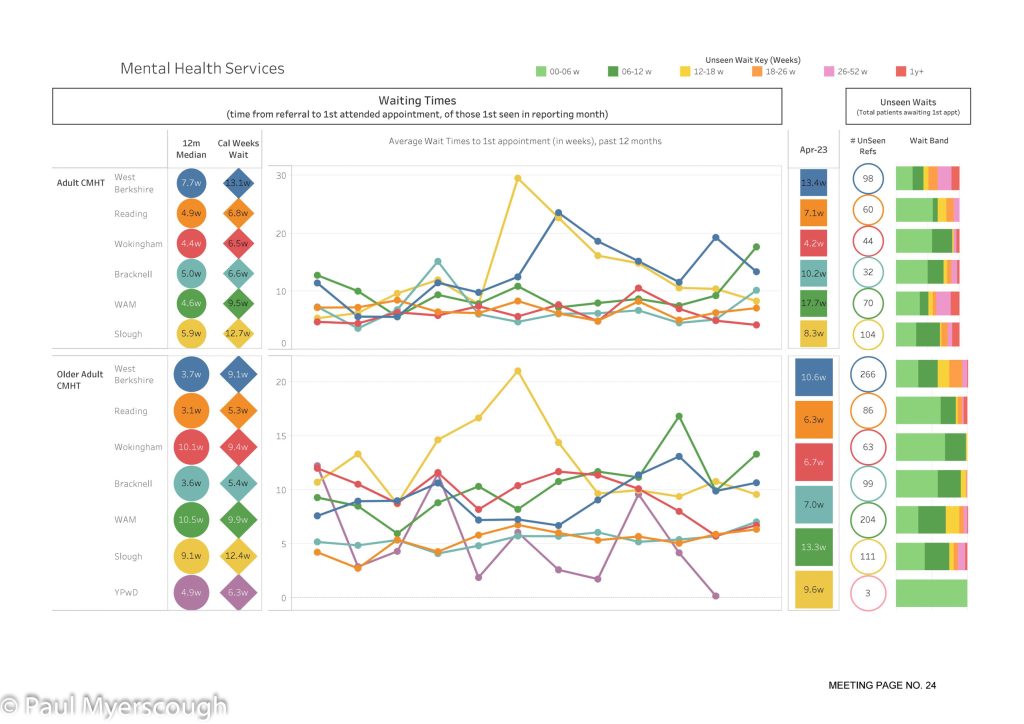
The examples above give an idea of the quality of waiting time information now available in BHFT. While it looks impressive there are caveats. First there are many services not yet covered by this report. Second, the report is only as accurate as the figures collected and reported by staff. A important factor in healthcare is ‘triangulation’, and so it is here. If a dataset is different for the same service in different parts of the county then there is reason to investigate, likewise if trends over time seem to be going in the wrong direction, or figures are at odds with service user feedback. Accurate or not, this report provides another tool for management to tackle the quality of services in the NHS.
One of the most important public documents on Trust performance is the annual Quality Account. NHS England define measures that must be documented. During my time we arranged for governors to preview the report and lodge questions before it was finalised. We also arranged several sessions with staff over a number of years on improving and augmenting the content. Governor comments and suggestions became a regular feature in an appendix at the back of the report. Many of the suggestions were implemented in the following year’s report. As a result the report itself has grown from just over 30 pages to more than 70, with the 30+ pages of appendices remaining about the same size. Now it rather a fine document – possibly one of the best introductions to the Trust. There were no governor comments for the 2022/23 report which suggests that it is now comprehensive and easy to understand. In recent years, as Lead Governor, I have produced a note to be included in the printed report and used this as a vehicle to lobby for changes such as an improved patient feedback mechanism and a renewed focus on carers.
The Trust Annual Report and Accounts is a rather dry document with the contents largely dictated by government. There is a section about governors which, to my knowledge has no input from governors themselves.
Trusts are required to consult governors on Trust Strategy. At the outset this was a difficult subject. A senior manager would have the role to coordinate the creation of a 3 year plan. In BHFT until recently those responsible were the King or Queen of Waffle. Questions about any subject were willingly answered, at length, until there was no time left in the meeting. Not only was the process vague, but objectives were often wishy-washy without clear measures. Specifying a time-line seemed to be a triumph. There was a strong sense that the consultation was a tick-box exercise with no recording of governor points and how they would be addressed.
Challenging Senior Managers in a governors meeting is not easy. But over the years I have persisted, and more recent plans show a better understanding about how to express objectives so that all stakeholders have a clear view on ambitions for the future. This, of course, is not a direct result of my personal interventions but I like to think governors input along with suitable management training has led to these gradual improvements.
Project Support
Governors are a good proxy for the public when it needs to be involved in Trust projects. From the outset I volunteered my services.
It didn’t always go smoothly. I was assigned as a member of the Steering Committee for the renewal of the Trust website. After two or three meetings I took along another governor colleague. He became a bit angry about some aspects of the the project. This upset the young team members and I was soon taken on one side by a senior manager – why we were present at that table when we were not welcome? Governors generally need not concern themselves with the detailed operation of the Trust.
One perennial concern for governors is the status and support of carers. Many of us believe that a carer who is with the patient every day can make all the difference to the outcome from therapy. Carers are empowered by the trained professionals who share their knowledge and provide a platform or place for carer support. Through this process the power of the clinical staff is multiplied.
When I became a governor the largest meetings I attended were the Carers Strategy meetings. With one or sometime two staff members from many of the 100 or so services that were asked to attend and explain their processes for Carers, the meetings seemed a bit chaotic. They were mostly for information sharing. There was no clear strategy from the top, so they were not very purposeful. The responsible manager was always en-route to a new role, which meant meetings were often cancelled.
One of my colleagues was a full time carer for her son and she doggedly pursued this subject and I supported her. When she ceased to be a governor I became a voice of the Carer. The Trust strategy never mentioned carers at first, but eventually the subject appeared. A manager was assigned to assess the status in the Trust and best practice; this resulted in a board proposal, and then a project. The project continues – producing standards and training materials and collecting and collating carer support information across the Trust. Now as a non-governor I still take an interest in this and attend the quarterly steering committee meetings.
From day one it was obvious to me that the standard NHS ‘Friends and Family’ test results did not contribute at all to service improvement. Time and again this was raised in meetings with staff and management. It was probably not governors which forced this issue into the open, so much as the Trust’s ‘QI Initiative’. This provided staff with basic training in some of the methods and cultures for process improvement. Once an organisation become conscious of QI, then customer (in our case, patient) feedback becomes an essential measure within the process.
While the Carers project is low-budget and low-key, creating a new process for collecting patient feedback is quite the opposite. Some of the governors participated in workshops with staff and many other stakeholders to determine the scope of this initiative. Consultants supported the exercise and produced a report to be used in a tender document. 3 companies bid to support the Trust in building the new processes and IT systems to support them.
Selecting a company and then moving the project forward in such a diverse organisation was no mean feat – especially for a project leader trained in occupational therapy and clinical staff management. The team producing the system for BHFT was rather small and, from my position as a member of the project steering committee, I was impressed by how they rose to the challenges which appeared month after month and took them in their stride. It was hard to see how they, as a company, could make a profit on this job. The Trust has named the process and system “I Want Great Care” (IWGC) after the name of the company that supported them.
Like all changes in the NHS this will take several years to completely bed in at all locations and across all services. But already the information dashboard at the heart of the system is showing areas where staff can improve their service to the patients.
Evaluating the performance of The Chairman
Our Chairman’s course had run out of time and we had to recruit a new one. What makes a good NHS Trust Chair? As Lead Governor and member of the A&R Committee, this was an important question. The current chair refused to help (‘not protocol’); the CEO did not answer emails about the subject; NHS providers wanted to help, but couldn’t; NHS-England didn’t exist but their predecessor organisation Monitor had nothing to say. The Kings Fund provided a board performance assessment matrix, which was relevant but not exactly the answer to my question. We managed, of course – quite well it seems. (More on this in the next instalment of this 3 part story – Part 3 “The Good, The Bad, and The Ugly”)
On Chair performance, however, whatever the prevailing view, this was not a subject for open discussion until about 5 years ago when NHS-England published some guidelines about performance assessment.
A facilitator is chosen – in our case one of the Non-Executive Directors – and their job is to solicit opinions from a wide range of stakeholders.
It is the Governors who appoint the Chair and in my view they must be satisfied that the evaluation is realistic. I spent several meetings with the facilitator helping her to adjust the process to meet our requirements. It is important to assess in a way which leads to performance improvement. On the first occasion the information collected was just blindly favourable and not helpful at all. In my (work) experience even the most senior executives have objectives set annually and I felt that our Chair should not be an exception. In the end it was my view that prevailed. Of course it is easy to set your own objectives so that you cannot fail, but that is another story!
Linking with Governors of other Trusts
For the NHS neophyte Berkshire Healthcare is so large and all-encompassing it is hard to look beyond its borders. But after a year or two I began to wonder how other Trusts approach governor issues.
Foundation Trusts fund an organisation called NHS-Providers (NHS-P) – a union for employers. This is the first stop for governor training on role and responsibilities. Each year NHS-P hosts a Governors Conference in London which provides an update on the management’s view of the NHS. All member organisations can send one or two governors. With several hundred colleagues in a room this is a good networking opportunity.
At one of these annual conferences several of us, Lead Governors at our Trusts, arranged to use a room in the venue after the main meeting. We set up a mailing group for exchanging information and resolved to consider the possibility of regional get-togethers for sharing best practice. We started by circulating a giant questionnaire which could serve to document differences in Trust practices up and down the country. Despite the large number of questions and high response level, there was remarkably little to learn. I used the group several times as a sounding board – on the use of technology for example, or the process of public engagement. There was no obvious best practice to pick up.
After several years the group has become the NLGA (National Lead Governors Association) with a constitution and a Chair, with about 60 or 70 members. New members regularly send questions to their colleagues and get some feedback about common practice. It can be reassuring to know that the challenges you see in your role have been considered by others and largely overcome by a better understanding of the governors role!
It was at the NHS-P conference that I met governors from 3 or 4 adjacent Trusts. Sporadic emails kept us in touch.
I had also attended one of NHS-P’s training courses. It covered the subject reasonably well, but group work seemed a little hollow with students, who were mostly new in their role, not knowing much about their Trusts. The shared learning was limited.
I discussed governor training with a new Company Secretary. She agreed to find out if NHS-P would come to us. This would enable new and experienced governors to work together on discussing our roles and responsibilities. I was also keen to involve governors from adjacent Trusts too – two trusts were contacted and invited to send governors along. One responded.

Two people from NHS-P came to deliver training about The Governor Role and Holding the Board to Account. This was a good session with useful information exchanged – not just the subjects brought by NHS-P. Some new relationships formed leading to further cooperation.
I arranged for BHFT governors to attend a Frimley Health governors meeting. This provided some insights for us in BHFT, about the technology used to support the meeting and about public engagement – their meeting also hosted members of the public with tea and cake. In practical terms however there was nothing to transfer to BHFT and the two or three colleagues who joined me did not feel a need to repeat the experience.
Another place where governors or Lead governors can come together for networking opportunities is provided by auditors. Most of the large audit firms have a health sector practice, and most of them audit several foundation trusts. From time to time I have been invited to a meeting in London with members from other Trusts. The focus is usually research coming from their health sector consultancy. This would often include information from other countries. Talking to other governors over break time, or after the main meeting was another opportunity to probe practices at other trusts.
There are some public conferences which provide a free place to NHS Trust governors. I attended a couple of these, but never found another governor there. These provide an opportunity to link up with some NHS luminaries but more likely it is commercial organisations that will ask for your business card!
In recent times there has been a new emphasis on ‘system working’ through the establishment of ICSs (Integrated Care Systems). Berkshire Healthcare belongs to two ICSs; one centred at Frimley to the East and the other to the West known as ‘BOB’ for Berkshire West, Oxfordshire, and Buckinghamshire. The good relationship with Frimley meant that information was shared early on through meetings to which governors were invited. BOB development took off more gradually and there seemed to be a reluctance to involve the public and participating Trust governors.
In response to this I worked with governor colleagues in neighbouring BOB Trusts to arrange a meeting with the new Chair of BOB ICS.
The BOB system and organisation was not developed at that time. Most positions in the organisation had not been filled and, obvious to me, communicating with the real actors in BOB must be a priority. Speculation and commitment about public consultation in the ICS could justifiably be postponed at this stage. The ICS does not deliver services directly to the public, these are provided by the Trusts and others in the ICS areas which already have their own public engagement strategies. My view was that Trust governors are not pre-eminent in discussion with ICS management and exist more-or-less as just another member of the public. My colleagues on the other hand felt there was a woeful disregard of their views and the voices of patients and there was a deliberate policy to bypass grass roots sentiments.
Generally speaking, because of the divergence of governor views and the frequent mis-apprehension of the governor role which by its nature should focus on the Trust and its area of operation, collaboration across Trusts between governors and Lead Governors is not usually a profitable activity.
Annual general Meeting
The Annual General Meeting (AGM) is a focal point in the Trust Calendar. It seems like a great opportunity to engage with the public – but without public engagement in many Trusts, those governors who describe it as a ‘box ticking exercise’ are correct.
In my early days I was impressed by how the Trust brought staff together at the AGM venue with stalls about their activities. There was always two services that presented interesting information about clinical initiatives. The room included staff, some governors, some ex-governors, and some local people. The Lead Governor made a few remarks followed by the CEO, and the Chief Finance Officer, before the two staff presentations.
Before long I was Lead Governor. Communication was important I thought. I restructured the Lead Governors report and catalogued the governor activities for the year, including a short assessment of the Trust from our point of view. For presentation I created a deck of Powerpoint slides. This explained what governor responsibilities were and some of what we had done during the year. It was designed for all governors to use in their public engagement activities – a concise way of explaining who they were as a representative of BHFT.
Each year I updated the material and presented it. I never received a question from the audience or feedback from governors or anyone else. I began to question who was there in the audience – the few faces seemed similar from year to year. Out of the 8-900,000 people in Berkshire who might use BHFT service, only 20 or fewer were attending the meetings.
After Covid we were to have a new experience – the AGM would be delivered online. This was exciting because potentially we could reach a much wider audience.
At the outset it was proposed that we filmed our parts so that they could be broadcast. As a governor, with no support or experience, this was not easy, but I eventually prepared something I was happy with. On the day of the AGM the Chair made his live introduction, then passed control to the Comms Team for my recording. They broadcast it without sound! 10 minutes of silence!
This was my last contribution to the AGM. The work involved in creating and presenting to a non-existing audience was too much for me. Making the AGM online gave ready access to our 5000 staff. The IT staff did not have the capability to identify any public members out of the 100 or so users attending the event.
A box-ticking exercise!
Next
Part three is provisionally called ‘The Good, The Bad, and the Ugly!’ and will include some comments about how effective the Governors Council in in NHS Foundation Trusts.